
Aero
A Hybrid Ventilation Machine That humanizes data Through Tangible-Digital Interaction:
Envisioning the Future of Anesthesia
Information
Umea Institute of Design
Partner: Maquet Getinge Group
Duration: 10 weeks
Medical, UX, System Design
Team: Shib Sahoo Shankar, Martina Eriksson
Role: Research & synthesis, ideation, prototyping/testing, documentation
Recognition
Tangible Embedded and Embodied Interaction Conference (TEI), Student Design Award: Stockholm Sweden 2018
Student Interaction Design Research Conference (SIDeR), Paper Presentation: Aalto, Finland, 2018
The context
Ventilation is an essential part of the anesthesia process during surgery. It requires the anesthesia nurse to make complex decisions to provide the patient with a safe and individualized ventilation experience.
The challenge
Data's loss of intrinsic meaning
When something as subjective as breathing is translated into numbers, its qualitative meaning is diluted. The current ventilation machine's GUI de-humanizes data and disassociates the patient from the data that is show in the GUI.
Non-intuitive
The current GUI also fails to utilize the full interaction potential between a human and machine, and is non intuitive in its control and interaction.
Cognitive Overload
Because anesthesia nurses currently uses statistical estimations and visual cues to set the patient's ventilation parameters, cognitive overload, and misinformed decisions become commonplace.
Patient Risk
These challenges in performing individualised ventilation can lead to partial lung collapse during pre-surgery intubation. This is called Atelectasis and affects 90% of people regardless of age, gender, health condition, or surgery duration.
How can we reduce cognitive overload, optimize human-machine interaction, and connect the nurse to the patient during anesthesia?
The Proposal

Aero: A Hybrid Ventilation Machine That Humanizes Data Through Tangible-Digital Interaction
Core function
Aero Assists The Nurse To Monitor The Patient, Make Assessments, And Perform Individualized Ventilation Care During Surgical Procedures.
Making Data Physical
We address the current GUI’s limitations by converting patient data into a more comprehensive, dynamic physical form.
patient breathing frequency
lung condition and pressure
Respiration graph translation
Tangible Data Manipulation
Through this expressive mode of data translation, ventilation can be controlled through tangible manipulation, also enabling the anesthesia nurse to connect with their patient.
Qualitative V. Quantitative
Quantitative data that requires more precise control is manipulated through the fine tuning dial on the perimeter of the TUI.



Aero’s Components
Aero’s System
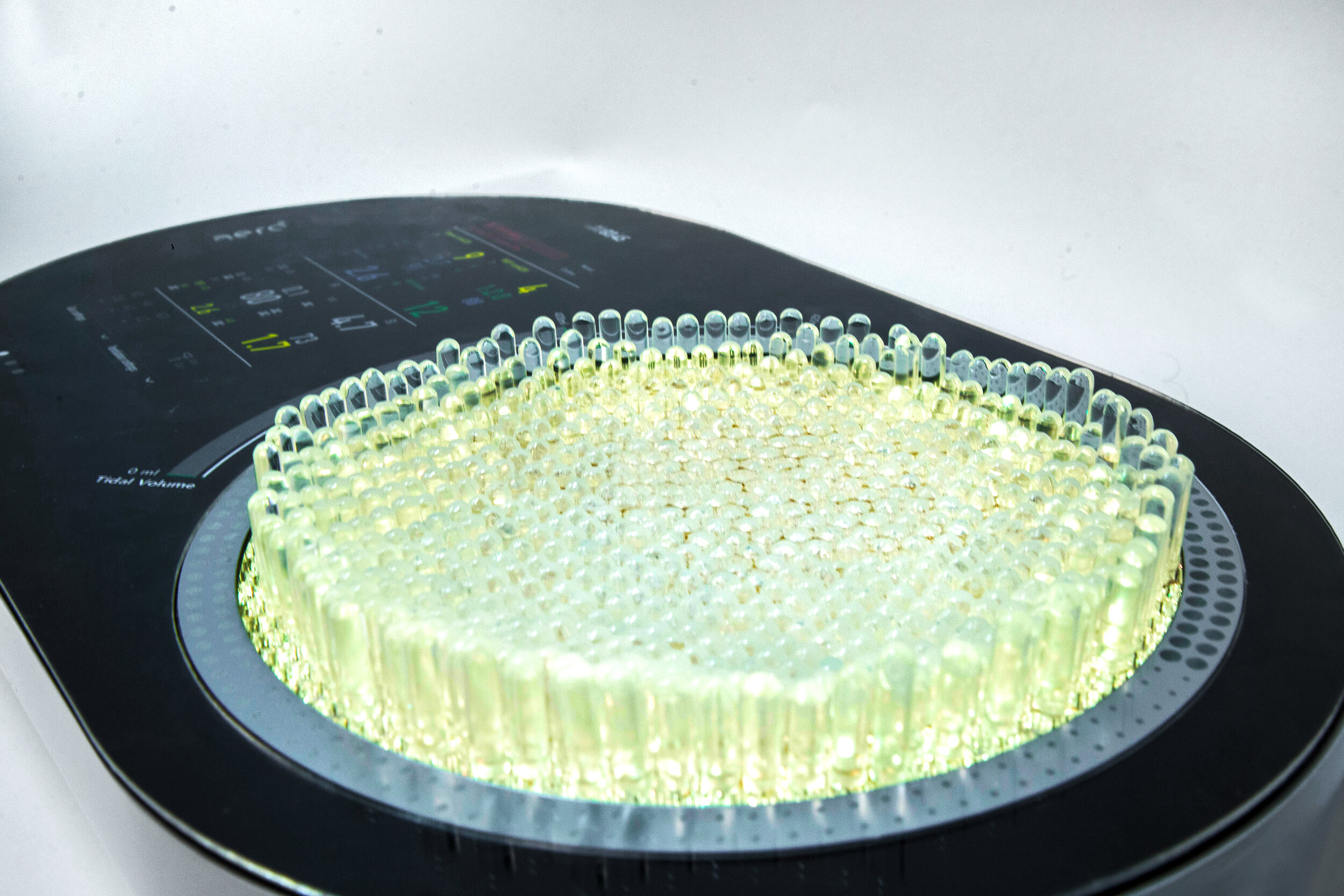
TUI Lung Pressure Expression
Aero's tangible user interface alerts nurse to patient lung condition through both physical form and color response. This expression allows for Peripheral Viewing as nurses multi-Task.
Normal Lung Pressure
Low Lung Pressure
High Lung Pressure
Process

Field Research
Prompt
How can we reduce cognitive overload, optimize human-machine interaction, and connect the nurse to the patient during anesthesia?
Locations
Umea General Hospital; ICU, Operating Room
Umea Emergency Station; Ambulance
Uppsala University Hospital; Operating Room
Methodologies
Expert interviews
Observation
Participatory learning
Research Synthesis
Operation timeline created to understand process of anesthesia and ventilation, in conjunction with the nurse’s responsibilities during surgery and in overall operating room system.
Initial preparation of anesthesia/ventilation procedure timeline
Digestion of research, operating room observations
Understanding net processes and relations in OR system
Journey mapping the patient journey
How is sleep depth and pain measured during surgery?
Mapping areas of interest with in emergency anesthesia + ventilation
Categorization
After initial expert interviews and synthesis, we divided our research into three areas of interest to create material for an initial co-creation/ideation workshop. This was followed by a validation workshop after ideas were refined to further develop and challenge the concepts.
Identifying Areas of Problem or Potential
After co creation and validation workshops and interviews, we took a deep dive into the topic of ventilation, identifying the following 5 areas. This helped us to determine the trajectory of our first ideation.
Ideation
How can we reduce cognitive overload, optimize human machine interaction, and connect the nurse to the patient?
Prototyping

Dual Interface Development
Quantitative versus Qualitative Data
Mapping manipulated, collected, and communicated data in the ventilation process.
Identifying qualitative and quantitative data.
Sketching form and movement
Exploration of Material, Data Expression, and Manipulation
Projection
Visual projection of anesthesia gas and oxygen flow within the lung
Can this give the anesthesia nurse qualitative information that accurately shows air distribution in the lungs?
Abstracted Fabric Lung
Responsive lung mimics respiration rate, and experiments with expression of movement.
Can this physicalized lung accurately represent patient lung condition? How can is respond to touch?
Jelly fish
Tangible resistance to simulate lung pressure and stiffness and give haptic feedback.
Can this method of tactile feedback give correlation between the data and patient to the nurse? Is there appropriate control through this direct manipulation?
Electronic + mechanical Components
Incorporating servo into prototype
Having fun!
Pressure-sensitive sighting
Refinement of Concept Direction + Hybrid Fusion of Prototypes
Mapping GUI and TUI relations, interactions.
Sketching of GUI architecture.
The Making of Aero

Prototype Building
Story boarding and Video Prep
Mapping our shot sequence to integrate the interaction, function, and user and patient journey in one cohesive and succinct narrative
Filming The Concept
A very generous nurse from research and concept validation phase participating in our video shoot, and helped to guide us to ensure it was accurate.















































